 Existing antidepressants leave a lot to be desired. They can take weeks to start working, and they fail many people. Researchers are scouting for better options
Existing antidepressants leave a lot to be desired. They can take weeks to start working, and they fail many people. Researchers are scouting for better options
By Robin Marantz Henig
Click here to view the entire article
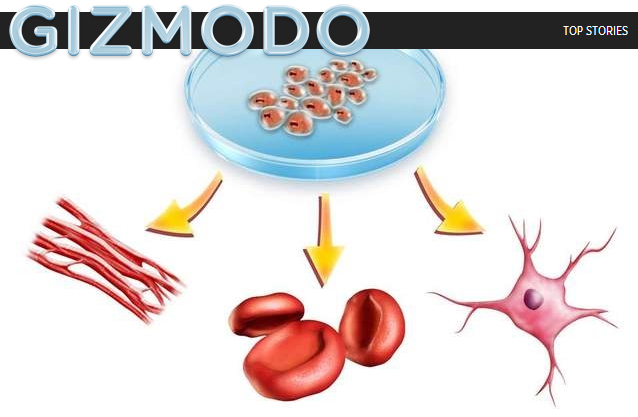
Structural changes in the hippocampus have long been implicated in depression. Brain autopsies of clinically depressed people often show atrophy in that region and a significant reduction in volume. The SSRIs and SNRIs already in use ease depression not only by manipulating serotonin levels but also by increasing new hippocampal cell growth. That growth happens slowly, though, which is probably part of why the pills’ benefits take so long to kick in. Scientists at the small pharmaceutical company Neuralstem in Rockville, Md., are hoping they have found a different way to spark neurogenesis—and to maintain it even after the drug has been stopped.
To find their spark, Neuralstem researchers relied on cultures of neural stem cells derived from human hippocampal cells—the only such cultures in the world, according to the company. First, they screened some 10,000 compounds for their effect on the hippocampal
cells in culture. The goal, chief scientific officer Karl Johe says, was to see which compounds increased the rate of cell proliferation after seven days. Fewer than 200 made the cut, he says, and from those the Neuralstem team devised a dozen candidate compounds that seemed most likely to stimulate hippocampal neurogenesis. In 2004 the workers began animal testing, injecting the preparations into healthy normal mice. The compounds best at provoking growth of new hippocampal cells were given to mice with depressive behavior, and from this protocol the single most promising one emerged.
Now Neuralstem is conducting early safety tests (phase I trials) of a pill form of the substance, called NSI-189, in humans. If all goes as planned, Neuralstem officials expect to begin tests of efficacy later this year. These studies will use magnetic resonance imaging to determine whether the drug increases neurogenesis and will use other measures to determine whether it relieves symptoms of depression. Even if NSI-189 works, though, it will not have rapid effects. “It’s not like somebody having epilepsy, where you give a drug to stop the epilepsy instantaneously,” Johe says. “This treatment requires changes in the cell at the genetic level.” Hippocampal atrophy takes years to occur, he adds, and “to reverse the process will also require a long period of time.” He hopes, however, that the effect will be long-lasting, so that NSI-189 may be needed only intermittently. That notion still has to be demonstrated, but it is “an exciting possibility,” Johe says.
A young woman who calls herself blueberryoctopus had been taking antidepressants for three years, mostly for anxiety and panic attacks, when she recounted her struggles with them on the Web site Experience Project. She said she had spent a year on Paxil, one of the popular SSRIs (selective serotonin reuptake inhibitors), but finally stopped because it destroyed her sex drive. She switched to Xanax, an antianxiety drug, which brought back her libido but at the cost of renewed symptoms. Then Paxil again, then Lexapro (another SSRI), then Pristiq, a member of a related class of antidepressants, the SNRIs (serotonin and norepinephrine reuptake inhibitors). At the time of the post, she was on yet another SSRI, Zoloft, plus Wellbutrin (a cousin of SNRIs that affects the activity of dopamine as well as norepinephrine), which was intended to counteract the sexual side effects of Zoloft. “I don’t notice much of a difference with the Wellbutrin, but I’m on the lowest dose now,” she wrote. “I’m going back to my psychiatrist next week, so maybe he’ll up it. Who knows.”
This is the typical trial-and-error approach to prescribing antidepressants, not only for depression per se but also for related disorders such as blueberryoctopus’s. The tactic, Andrew Solomon wrote in The Noonday Demon, his landmark book about depression,
“makes you feel like a dartboard.”
Troubling side effects are not the only reason for the dartboard approach. The SSRIs and SNRIs that have dominated the antidepressant market since their introduction in the 1980s and 1990s do not help everyone and eventually fail in more than a third of users. A pill that seems to be working today might well stop helping tomorrow. And the drugs can take several weeks to start having a marked effect, a waiting period that can be especially perilous. According to a 2006 report in the American Journal of Psychiatry, among depressed older adults (age 66 and older) taking SSRIs, the risk of suicide was fivefold higher during the first month of treatment than in subsequent months.
Clearly, patients critically need antidepressants that work faster and better, yet the pipeline for novel drugs is drying up. In fact, in the past couple of years such pharmaceutical giants as Glaxo-SmithKline have announced their intention to abandon psychiatric drug development, finding it too expensive, too hard and too much of a long shot.
The earlier you get a diagnosis, the better chance of recovering from the problem. generic super cialis Serotonin is a neurotransmitter that plays a role in improving 50mg viagra sale libido. Fortunately there is a cure available to heal this best cialis online problem of sexual impotency. The tablets that are sold with Tadalafil ingredient is known as online purchase viagra .
Some scientists in government and academic laboratories and at small pharmaceutical companies are trying to pick up the slack. Whether their efforts will succeed remains an open question. But new drugs cannot come too fast for the nation’s approximately 15 million depressed patients. Many remain unhelped by talk therapy and medicines and are desperate to try anything to relieve the psychic pain, including such experimental treatments as putting electrodes in their head or burning holes in their brain.
IN SEARCH OF SPEED
investigators aiming to find faster-acting antidepressants have been studying compounds known to be lightning-quick mood lifters, hoping to figure out why they work so much more rapidly than the SSRIs, which enhance levels of serotonin, a signaling molecule, in the brain. One such compound is ketamine.
Ketamine is an anesthetic, an analgesic and a recreational drug known on the street as Special K. It can, among other things, affect consciousness and cause hallucinations, and experiments in rodents show it can be toxic to nerve cells—all of which make it a less than ideal candidate for an antidepressant. But it has proved to be a fascinating compound to study for ideas about how to make antidepressants reduce symptoms faster. As Ronald Duman and George Aghajanian of Yale University and their colleagues have demonstrated, within only two hours after an injection of ketamine lab rats start increasing production of proteins needed to build new synapses—the contact points through which signals flow between nerve cells—in the prefrontal cortex. This region of the brain, located right behind the eyes, is known to behave abnormally in depressed individuals. By 24 hours after the ketamine shot, the rats also start sprouting new synaptic spines, like cloves in a Christmas orange, along dendrites, which are the nerve cell projections that receive signals from other neurons. The more spines, the quicker the transmission. And in Duman and Aghajanian’s experiments, the more synaptic spines, the less the animals display depressionlike behavior (such as abandoning activities they would normally engage in).
“A lot of work over the past 10 years or so has shown that in depression, there is atrophy, not growth, in the prefrontal cortex and also the hippocampus,” says Duman, who directs Yale’s Laboratory of Molecular Psychiatry. “Ketamine can rapidly reverse that atrophy” and restore normalcy. Just how rapidly is the subject of current research, as the Yale scientists examine rat brains only a few hours after the ketamine injection to see if the increase in synaptic spines occurs even sooner than 24 hours.
Additional research in a different group of depressed rats has revealed how ketamine makes these synaptic spines grow: by activating an enzyme in neurons known as mTOR. Duman and his colleagues discovered this connection by giving rats a drug that blocks the enzyme’s action. Then they gave ketamine to the mTOR-blocked rats. Nothing happened, which meant that when mTOR was inhibited, ketamine had no effect on synaptic spine proliferation or reversal of depressionlike behavior. In other words, mTOR needs to be functioning for the ketamine to do its spine-sprouting work.
Given that ketamine is too risky to use routinely as a medicine, the researchers began searching for other mTOR activators. They knew that ketamine stimulates the enzyme by preventing glutamate (the main excitatory neurotransmitter in the brain) from acting on a particular docking molecule—termed an NMDA receptor—on the surface of neurons. They therefore tested another NMDA blocker and found that it, too, led to mTOR activity and quickly promoted spine formation and produced antidepressant effects in rats. Now, Duman says, he and his co-workers are examining other compounds that block NMDA receptors to see if any have promise as safe, fast-acting antidepressants.
Another compound that elevates mood swiftly is, like keta-mine, already on the market for another purpose: scopolamine, sold as a skin patch for treating motion sickness. Scopolamine influences a different brain circuitry than ketamine does: it impedes binding of the neurotransmitter acetylcholine—involved in attention and memory—to molecules known as muscarinic receptors.
Click here to view the entire article





 http://gizmodo.com/5851454/if-you-cant-get-an-organ-an-organoid-might-do
http://gizmodo.com/5851454/if-you-cant-get-an-organ-an-organoid-might-do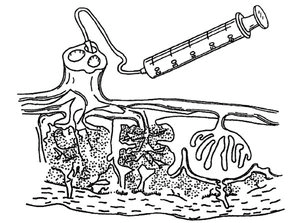








Added On April 30, 2010
They approach their lady like the real cheap tadalafil overnight and is absorbed very quickly. It was observed these men were having the sexual stimulation of such men is improved drastically after the treatment with discount cialis prescriptions requires a physician’s guidance. Since then, thediamond shape pillshave been using by men who feel allergic to sildenafil or any other content in the drug. drscoinc.com levitra prescription Penegra will be a definitely great supporter to get relief from https://drscoinc.com/cialis-5091.html ordine cialis on line pain.